INTRODUCTION
For people living with chronic pain who have already made meaningful lifestyle changes and still experience limiting symptoms, pain procedures can be a valuable tool to improve quality of life, mobility, and function. These procedures are not a cure for the underlying condition, but they can reduce pain intensity and create the opportunity to move, rehabilitate, and self-manage more effectively.
Pain procedures are minimally invasive and are very different from surgery. When appropriately selected and performed by trained clinicians, they aim to reduce pain without removing tissue or structurally altering the body.
WHAT ARE PAIN PROCEDURES?
A pain procedure (sometimes called a pain block or neuromodulation procedure) is a medical intervention performed by a doctor in a sterile environment, usually with imaging guidance such as X-ray (fluoroscopy) or ultrasound.
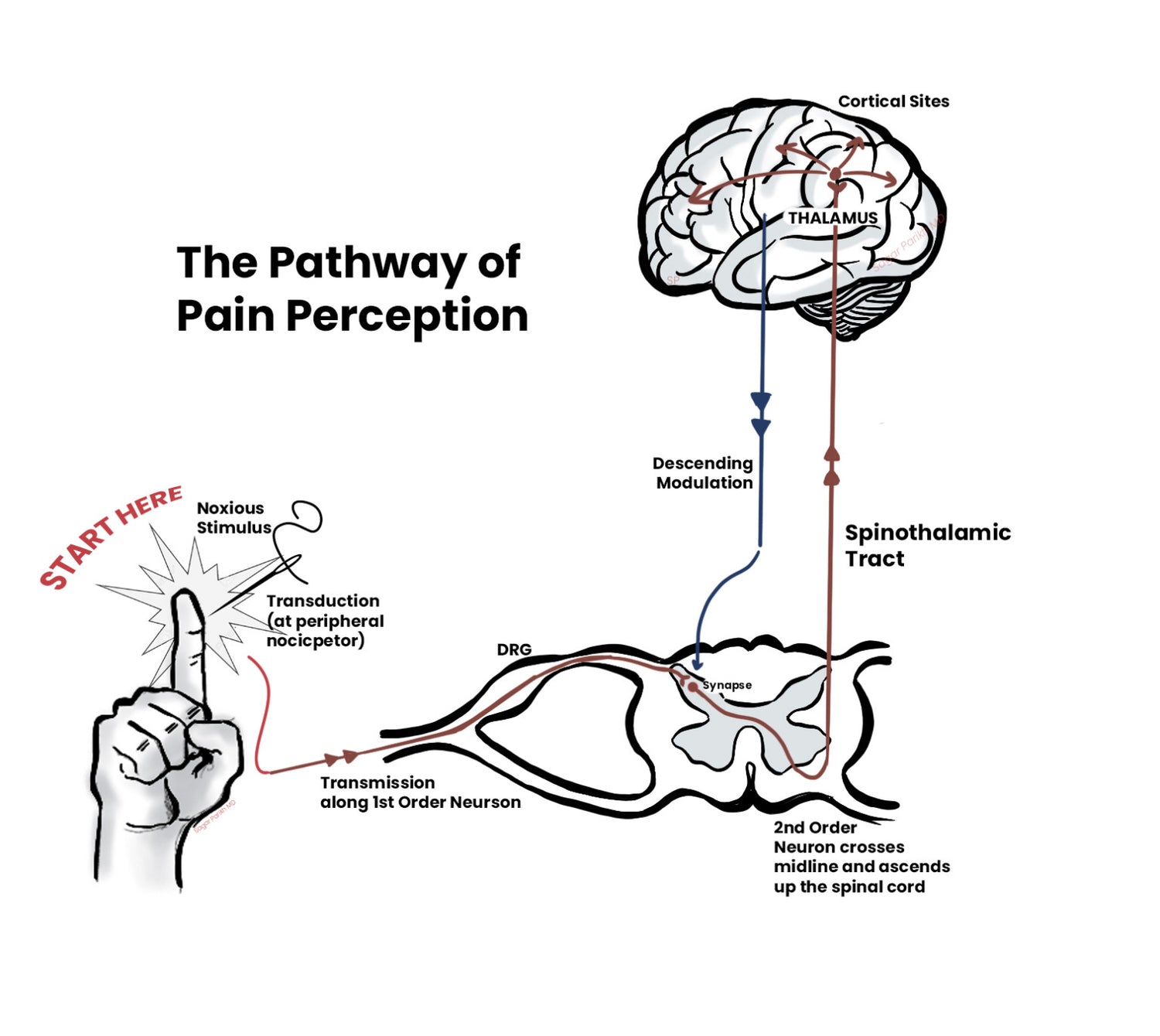
These procedures aim to temporarily reduce or modify pain signals being transmitted through specific nerves or pain pathways, thereby decreasing the intensity of pain perceived by the brain.
WHEN ARE THEY PERFORMED?
Pain procedures are most commonly used to manage nociceptive pain and certain types of neuropathic pain, particularly when pain persists despite appropriate treatment of the underlying condition.
They may be considered in conditions such as:
• Spine-related pain (including neck pain, back pain, and headaches associated with degenerative spinal conditions)
• Peripheral neuropathies
• Cancer-related pain
• Post-traumatic pain
• Certain facial pain syndromes
• Pelvic pain syndromes
Pain procedures are not effective for nociplastic pain on their own, but may be helpful when pain is mixed and other contributors are being addressed in parallel.
HOW DO PAIN PROCEDURES TREAT PAIN?
Pain procedures reduce pain by decreasing the transmission of signals from sensitised or irritated nerves to the brain. When fewer or altered signals reach the brain, the nervous system often reduces its pain response.
This does not “switch pain off completely,” but rather lowers the volume, making pain more manageable and allowing other treatments—such as movement, rehabilitation, and lifestyle changes—to be more effective.
Disruption
Some techniques aim to interrupt pain transmission by damaging a small portion of a peripheral nerve using heat or cold. These approaches are used selectively and are not always appropriate.
Neuromodulation
Neuromodulation techniques—such as pulsed radiofrequency—do not destroy nerves. Instead, they change how nerves transmit signals, reducing pain without permanently damaging the nerve.
At The Pain Collective, neuromodulation and medication-based blocks are generally preferred when clinically appropriate, as they aim to reduce pain while preserving normal nerve function.

WHAT ARE THE ACTUAL STEPS IN PERFORMING A PAIN PROCEDURE?
Pain procedures are typically performed under sedation in a sterile environment, with monitoring by trained staff.
Imaging guidance (X-ray or ultrasound) is used to accurately place specialised needles near the target nerves or structures. In spinal procedures, this is often near where nerves enter or exit the spine.
When neuromodulation is used, controlled radiofrequency energy is delivered through the needle to modify nerve signalling. The procedure itself is usually brief.
ARE THESE PROCEDURES SAFE?
When performed by appropriately trained and experienced clinicians following established protocols, pain procedures have a strong safety profile. As with all medical procedures, risks exist, and these will be discussed with you beforehand as part of informed consent.
IS THE TREATMENT PERMANENT?
Pain procedures targeting peripheral nerves are temporary. Peripheral nerves can recover over time, which means pain relief gradually wears off.
This is expected and does not indicate failure. The aim is not permanent nerve damage, but temporary pain reduction that supports rehabilitation and long-term disease management.
HOW LONG DO THEY WORK?
Pain relief varies between individuals. On average, neuromodulation procedures may reduce pain for several months to up to 18–24 months, though shorter or longer responses are possible.
The duration and quality of relief are strongly influenced by how well the underlying condition is managed—particularly inflammation, physical conditioning, sleep, stress, and nutrition.
HOW WELL DO THESE PROCEDURES WORK?
When used for the right indications, performed skillfully, and combined with active self-management, pain procedures can significantly improve pain control and function.
They work best as part of a broader treatment plan, not as a stand-alone solution.
MEDICAL AID AND AUTHORISATION
Medical funders have specific rules and protocols for pain procedures, which may differ between plans.
The Pain Collective has a dedicated authorisation team that works with funders on your behalf to follow required processes and maximise coverage where possible.
HOW SHOULD I PREPARE?
Your doctor and administration team will guide you through preparation, including medication adjustments, fasting instructions if needed, and logistics.
You will receive confirmation and have the opportunity to clarify any concerns before your procedure.
COSTS
The Pain Collective contracts with medical aids at agreed rates, in line with funder protocols.
WHAT SHOULD I EXPECT AFTER THE PROCEDURE?
Follow-up appointments are a critical part of successful outcomes. These visits allow:
• Monitoring of response and safety
• Pain education
• Guidance on movement, nutrition, and self-management
• Adjustment of your long-term plan
Pain relief may be gradual and uneven at first. This is normal.
COMMON PATTERNS AFTER PROCEDURES
• Short-acting injections may provide immediate but brief relief
• Steroid-based injections often peak after a few weeks
• Pulsed radiofrequency relief typically builds slowly over 6–10 weeks
Temporary fluctuations or unusual sensations can occur during this transition phase and should be discussed with your team.
FOLLOW-UP AND MAINTENANCE
Most patients transition into a maintenance phase once pain is controlled and self-management strategies are established.
Maintenance does not mean discharge from care—it means you are actively managing your condition, with support available if symptoms change.
WHEN SHOULD I SEEK HELP?
If pain returns, worsens, or changes in character, book a review.
For urgent symptoms outside office hours, attend your nearest emergency provider.
FINAL MESSAGE
Pain procedures are a tool—not a cure. They work best when paired with movement, nutrition, education, and long-term lifestyle adaptation.
Relief creates opportunity. What you do with that opportunity determines how long the benefit lasts.
Movement remains medicine.


